What are the Different Stages of Esophageal Cancer?
Esophageal cancer is a formidable disease that affects the esophagus, the hollow tube that carries food and liquids...
+919999461292
MBBS | DNB (General Surgery, Gold Medalist) | DNB (Thoracic Surgery, Gold Medalist)
Thoracic & Lung Transplant Surgeon | Medanta – The Medicity, Gurugram

MBBS | DNB (General Surgery, Gold Medalist) | DNB (Thoracic Surgery, Gold Medalist)
Thoracic & Lung Transplant Surgeon | Medanta – The Medicity, Gurugram

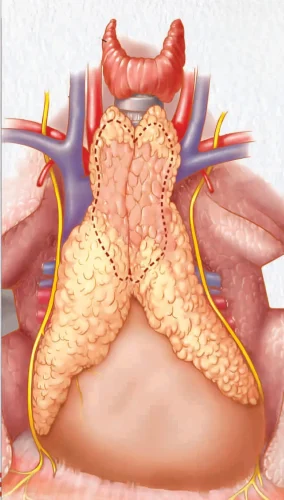
Myasthenia gravis (MG) is an autoimmune neuromuscular disorder characterized by muscle weakness and fatigue, while thymoma is a tumor originating from the thymus gland. These two conditions are closely linked, as they can coexist and influence each other. The treatment of myasthenia gravis and thymoma requires a multidisciplinary approach, involving neurologists, oncologists, and surgeons, to address both the neurological symptoms and the underlying tumor. Understanding the interplay between MG and thymoma is crucial for effective management and improved patient outcomes
See, about 10-15% of Myasthenia Gravis patients have thymoma – that’s tumor in thymus gland. Sometimes treating thymoma can actually improve Myasthenia symptoms. They’re like connected problems, you understand?”
Actually, we need to manage both conditions together. First we’ll stabilize your Myasthenia symptoms with medicines, then plan thymoma surgery when you’re stable. It’s like preparing ground before building house.
In most cases, yes. We do minimally invasive surgery called VATS thymectomy. Very small cuts, faster recovery. But sometimes we might need other treatments like radiation also, depending on tumor stage.
There are some special considerations, but we take extra precautions. We’ll work with neurologist to optimize your condition before surgery. Our anesthesia team is very experienced in handling such cases.
You’ll need to continue your Myasthenia medicines initially. We’ll gradually adjust doses based on your symptoms. Some patients eventually need less medication, but changes must be done slowly and carefully.
Usually 5-7 days after surgery. First few days in ICU for close monitoring, then shift to room. We need to make sure your Myasthenia symptoms are stable before discharge.
Main things – take medicines regularly, attend all follow-ups, avoid stress, maintain good sleep pattern. Also very important to monitor and report any new symptoms immediately.
Start with gentle exercises after 6 weeks. Gradually increase as tolerated. Listen to your body – if feeling tired, take rest. We’ll guide you about proper exercise program.
No strict restrictions, but healthy, balanced diet is important. Some medicines need to be taken before food, some after – we’ll give proper schedule. Stay well hydrated always.
First month every week, then monthly for 3 months. After that, every 3 months if stable. We’ll coordinate with your neurologist for combined follow-up.
Watch for increased muscle weakness, difficulty swallowing, breathing problems, or fever. If any of these occur, contact us immediately. Better safe than sorry.
Once stable, yes. But first 3 months, stay close to hospital. Always carry your medicines, medical records. Inform us before planning long trips.
Initially you’ll need good rest. Most patients return to desk jobs in 6-8 weeks. Physical jobs might need longer. We’ll help plan your return to work appropriately.
With proper treatment, most patients manage well. Regular follow-up, medication compliance, and lifestyle modifications are key. Many lead normal, active lives.
Note: “Remember, treating these conditions needs teamwork between you, me, and the neurologist. Good communication is very important. Don’t hesitate to contact us with any concerns.”
Esophageal cancer is a formidable disease that affects the esophagus, the hollow tube that carries food and liquids...
Esophageal cancer is a formidable and often challenging disease that affects the esophagus, the muscular tube that carries...
Esophageal cancer is a challenging and potentially life-threatening condition that requires timely diagnosis and appropriate treatment. When esophageal...
Esophageal cancer is a serious and potentially life-threatening disease that affects the esophagus, the muscular tube that carries...
Esophageal cancer is a formidable adversary that can silently develop within the esophagus, the muscular tube connecting the...
Esophageal cancer is a serious and potentially life-threatening condition that affects the esophagus, the muscular tube responsible for...
WhatsApp us