What are the Different Stages of Esophageal Cancer?
Esophageal cancer is a formidable disease that affects the esophagus, the hollow tube that carries food and liquids...
+919999461292
MBBS | DNB (General Surgery, Gold Medalist) | DNB (Thoracic Surgery, Gold Medalist)
Thoracic & Lung Transplant Surgeon | Medanta – The Medicity, Gurugram

MBBS | DNB (General Surgery, Gold Medalist) | DNB (Thoracic Surgery, Gold Medalist)
Thoracic & Lung Transplant Surgeon | Medanta – The Medicity, Gurugram


Tracheal Stenosis: Understanding a Narrowed Windpipe
Tracheal stenosis is a medical condition characterized by the narrowing of the trachea, the main airway that connects the larynx (voice box) to the lungs. This narrowing can restrict the flow of air into and out of the lungs, leading to breathing difficulties and other respiratory symptoms. Tracheal stenosis can result from various causes, and understanding its pathophysiology, clinical presentation, diagnosis, and treatment is essential for effective management and improved patient outcomes.
See, Tracheal Stenosis is basically narrowing of your windpipe. Think of it like water pipe becoming narrow at some point. This makes breathing difficult because less air can pass through.
Most common causes are prolonged intubation, previous throat surgery, wind-pipe tumors or some injury to throat. Sometimes it can happen from infections also. In your case, we’ll need to find exact cause.
It can be quite serious if left untreated because it affects your breathing. But don’t worry too much – we have very good treatment options nowadays. Success rates are quite encouraging.
Depending on severity, we have different options – sometimes we can do endoscopic dilation, sometimes we need surgery. Please contact me and send your reports, we will decide the appropriate plan for you.
Not always immediate. First we’ll do proper evaluation with breathing tests and scans. Sometimes we try conservative treatment first. We’ll decide best approach for your condition.
Usually takes 2-3 hours. In surgery, the diseased portion of the trachea is removed and the normal tracheal is re-connected to the normal trachea part. In simple words, if a portion of the water-pipe is damaged you are removing that portion and re-joining the normal portions. As I said, this looks very simple but requires a very good experienced team to perform it very diligently. We use advanced techniques to repair stenosis and we have the highest experience in managing such problems.
Typically patients stay in hospital for 5-7 days. Complete recovery takes about 4-6 weeks. But you’ll start noticing breathing improvement immediately after surgery.
Voice actually improves after surgery. However, there might be temporary voice changes, but usually returns to normal in a few days. If needed, we’ll arrange speech therapy sessions.
Main things to watch – breathing difficulty, excessive coughing, fever, or throat pain. If you notice any of these, contact us immediately. But complications are quite rare with proper care.
Most patients return to desk job in 3-4 weeks. Physical work might need 6-8 weeks. We’ll assess your recovery and guide accordingly.
Can start with gentle walking from next day after surgery. Gradually increase activity. No heavy exercise for 2-3 months. We’ll give you a proper exercise plan based on your recovery.
For few days after surgery all food will be given through a pipe,not from mouth. This is because the swallowing mechanism will take some time to come to normal state after surgery. Till the time it recovers, this tube feeding will help you to maintain the nutrition. Within a week or 10 days, once the normal swallowing mechanism recovers, we can start oral diet. Initially soft diet is better. Avoid very hot or cold foods. Small, frequent meals are good. We’ll give detailed diet instructions before discharge.
First month weekly, then monthly for 3 months. After that, every 6 months if everything stable. But if any problems develop, contact immediately.
Recurrence is a rarity after proper surgery if all the surgical principles are followed. Regular follow-up helps catch any problems early. Following post-treatment instructions is very important.
No smoking absolutely, avoid dusty environments, maintain good throat hygiene. Regular breathing exercises help. We’ll teach you specific techniques.
Note: Remember, proper follow-up and following instructions carefully is very important for good recovery. My team and I are always here to help if you have any concerns.
Tracheal Stenosis: Understanding a Narrowed Windpipe
Tracheal stenosis is a medical condition characterized by the narrowing of the trachea, the main airway that connects the larynx (voice box) to the lungs. This narrowing can restrict the flow of air into and out of the lungs, leading to breathing difficulties and other respiratory symptoms. Tracheal stenosis can result from various causes, and understanding its pathophysiology, clinical presentation, diagnosis, and treatment is essential for effective management and improved patient outcomes.

The trachea, also known as the windpipe, is a rigid, tube-like structure that starts just below the larynx and extends into the chest, where it divides into the right and left main bronchi, leading to the lungs. The trachea is composed of C-shaped cartilage rings connected by fibrous tissue and smooth muscle. This unique structure allows the trachea to remain open for airflow while still providing flexibility for swallowing and neck movement.
The primary function of the trachea is to transport air to and from the lungs during the process of breathing. It acts as a conduit for the exchange of oxygen and carbon dioxide, playing a vital role in the respiratory system.
Tracheal stenosis can be classified as congenital or acquired, depending on its underlying cause:
– Congenital Tracheal Stenosis: This type of stenosis is present at birth and results from abnormal development of the trachea during fetal growth. It can be caused by factors such as genetic mutations, prenatal infections, or intrauterine trauma.
– Acquired Tracheal Stenosis: Acquired stenosis occurs after birth and can result from various factors, including:
a) Trauma: External injuries or internal trauma to the trachea, such as a direct blow to the neck or a penetrating injury, can cause scarring and narrowing of the airway.
b) Endotracheal Intubation: Prolonged intubation with a breathing tube, as is often done during surgery or in the intensive care unit, can lead to tracheal damage and subsequent stenosis.
c) Infections and Inflammatory Conditions: Conditions such as prolonged intubation with a breathing tube, as is often done during surgery or in the intensive care unit, can lead to tracheal damage and subsequent stenosis.
d) Autoimmune Disorders: Certain autoimmune diseases, such as relapsing polychondritis, can cause inflammation of the tracheal cartilage, leading to stenosis.
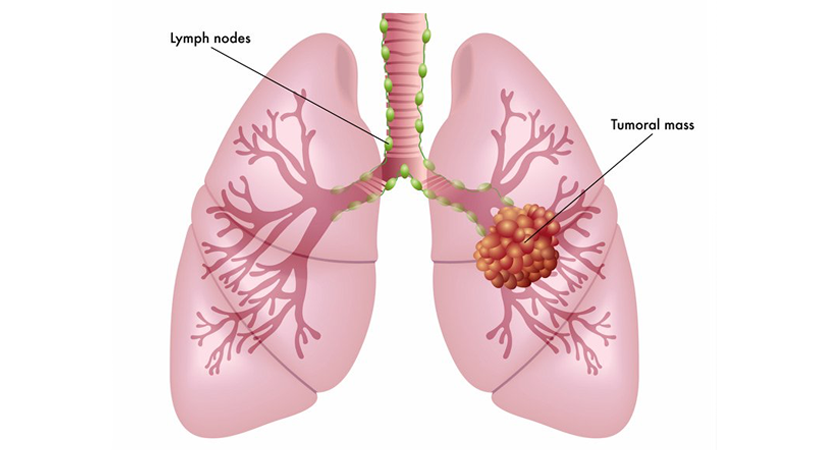
e) Tumors: Benign or malignant growths in or around the trachea can compress the airway and cause narrowing.
f) External Compression:** Compression of the trachea by structures outside the airway, such as an enlarged thyroid gland or a mediastinal mass, can also result in stenosis.
The symptoms of tracheal stenosis can vary depending on the degree of narrowing and the underlying cause. Common signs and symptoms may include:
– Shortness of breath (Dyspnea): Breathing becomes difficult and may be accompanied by a feeling of suffocation.
– Wheezing: A high-pitched whistling sound during breathing due to narrowed air passages.
– Stridor: A harsh, noisy breathing sound that occurs during inspiration and is often a sign of significant tracheal narrowing.
– Chronic Cough: A persistent cough may be present, especially if there is irritation of the airway.
– Recurrent Respiratory Infections: Tracheal stenosis can compromise the body’s ability to clear mucus and debris, leading to an increased risk of respiratory infections.
– Cyanosis: Bluish discoloration of the skin and mucous membranes due to reduced oxygenation of the blood.
– Exercise Intolerance: The limited airflow can lead to fatigue and shortness of breath with physical activity.
In severe cases, tracheal stenosis can lead to life-threatening respiratory distress, especially during periods of exertion or stress.
The diagnosis of tracheal stenosis starts with a thorough medical history and physical examination, paying close attention to respiratory symptoms and risk factors. Diagnostic tests and imaging studies may be ordered to confirm the diagnosis and assess the severity of the stenosis:
– Pulmonary Function Tests (PFTs): These tests measure lung function and airflow, helping to identify any significant respiratory abnormalities.
– Chest X-ray: X-ray imaging can provide initial information about the tracheal anatomy and any potential masses or compressions.
– Computed Tomography (CT) Scan: CT scans offer detailed cross-sectional images of the trachea, allowing the physician to assess the degree and extent of stenosis.
– Bronchoscopy: This is a crucial diagnostic tool for directly visualizing the trachea and airways. A flexible bronchoscope is inserted through the nose or mouth and passed into the trachea, allowing the physician to visualize any stenotic areas and take tissue samples if needed.
Tracheal stenosis is classified based on its location and extent within the trachea:
– Subglottic Stenosis: Narrowing of the trachea just below the level of the vocal cords (glottis). This type can result from intubation injury or autoimmune conditions.
– Tracheal Stenosis: Stenosis involving any part of the trachea, from the level of the glottis to the division of the main bronchi.
– Tracheobronchial Stenosis: Narrowing that extends into the bronchi, the smaller airways leading to the lungs.
The management of tracheal stenosis depends on its severity, location, and underlying cause. Treatment options include:
– Medical Management: Mild cases of tracheal stenosis may be managed conservatively with medications to alleviate symptoms and treat any underlying infections or inflammation.
– Endoscopic Interventions: For certain types of tracheal stenosis, endoscopic techniques may be used to dilate the narrowed airway and place stents to keep it open.
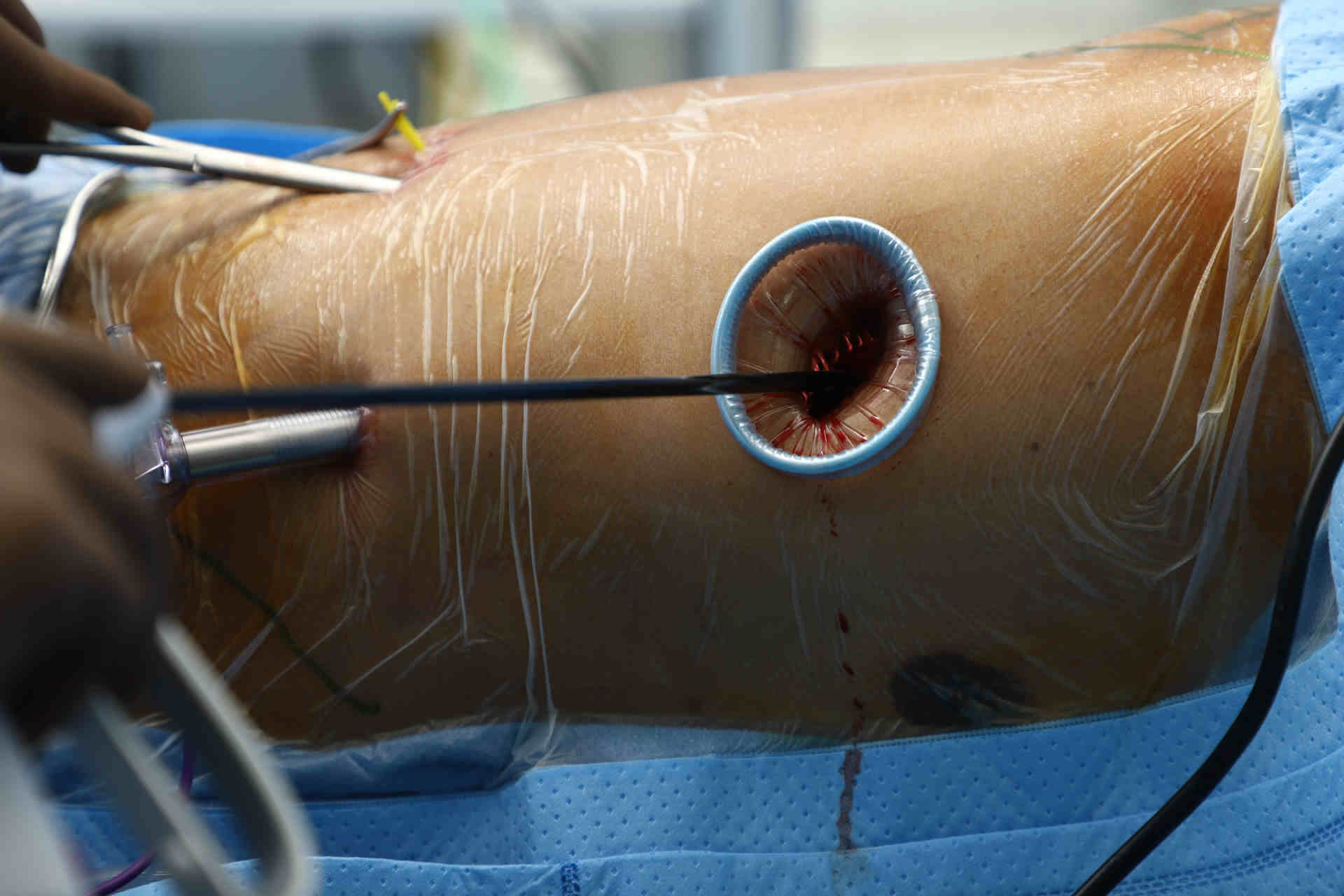
– Surgical Interventions: In more severe cases or when endoscopic methods are not sufficient, surgical procedures may be necessary to repair or reconstruct the trachea. Surgical options include tracheal resection and anastomosis, laryngotracheal reconstruction, or tracheal transplantation.
– Tracheostomy: In cases where the trachea is severely compromised and other interventions are not feasible, a tracheostomy may be performed. This involves creating a surgical opening in the neck to insert a breathing tube directly into the trachea.
The prognosis for individuals with tracheal stenosis depends on the extent of the narrowing, the presence of any associated medical conditions, and the response to treatment. Mild cases may be effectively managed with conservative measures, while more severe stenosis may require surgical interventions.
Complications of tracheal stenosis can include recurrent respiratory infections, respiratory distress, and worsening respiratory function. Prompt diagnosis and appropriate management are crucial for preventing complications and improving long-term outcomes.
After treatment for tracheal stenosis, rehabilitation and follow-up care are essential for optimizing recovery and monitoring the airway’s health. Individuals may require pulmonary rehabilitation to improve lung function and enhance exercise tolerance. Regular follow-up visits with healthcare providers are necessary to assess the airway’s patency and address any potential complications or recurrence.
Advancements in medical technology and research continue to drive the development of new therapies for tracheal stenosis. Innovative approaches, such as tissue engineering and regenerative medicine, hold promise for enhancing tracheal reconstruction and improving outcomes for individuals with severe stenosis.
While congenital tracheal stenosis may not be preventable, certain measures can reduce the risk of acquired stenosis:
– Proper Intubation Techniques: Healthcare providers should adhere to best practices for endotracheal intubation and closely monitor patients undergoing prolonged intubation to minimize the risk of tracheal damage.
– Early Detection and Treatment: Prompt identification and management of respiratory infections, autoimmune conditions, and other potential risk factors can help prevent the development of tracheal stenosis.
Esophageal cancer is a formidable disease that affects the esophagus, the hollow tube that carries food and liquids...
Esophageal cancer is a formidable and often challenging disease that affects the esophagus, the muscular tube that carries...
Esophageal cancer is a challenging and potentially life-threatening condition that requires timely diagnosis and appropriate treatment. When esophageal...
Esophageal cancer is a serious and potentially life-threatening disease that affects the esophagus, the muscular tube that carries...
Esophageal cancer is a formidable adversary that can silently develop within the esophagus, the muscular tube connecting the...
Esophageal cancer is a serious and potentially life-threatening condition that affects the esophagus, the muscular tube responsible for...
MBBS | DNB (General Surgery, Gold Medalist) DNB (Thoracic Surgery, Gold Medalist)
Thoracic & Lung Transplant Surgeon
Medanta – The Medicity, Gurugram
An esteemed thoracic surgeon, excels in minimally invasive procedures (VATS & Robotic surgery) for both benign and malignant lung conditions. With a stellar academic background and international training, he is dedicated to offering compassionate and expert patient care.

Website Engineered with ❤️ by GigaWebZone, a leading web development company.
Copyright © 2025 All rights reserved.
WhatsApp us