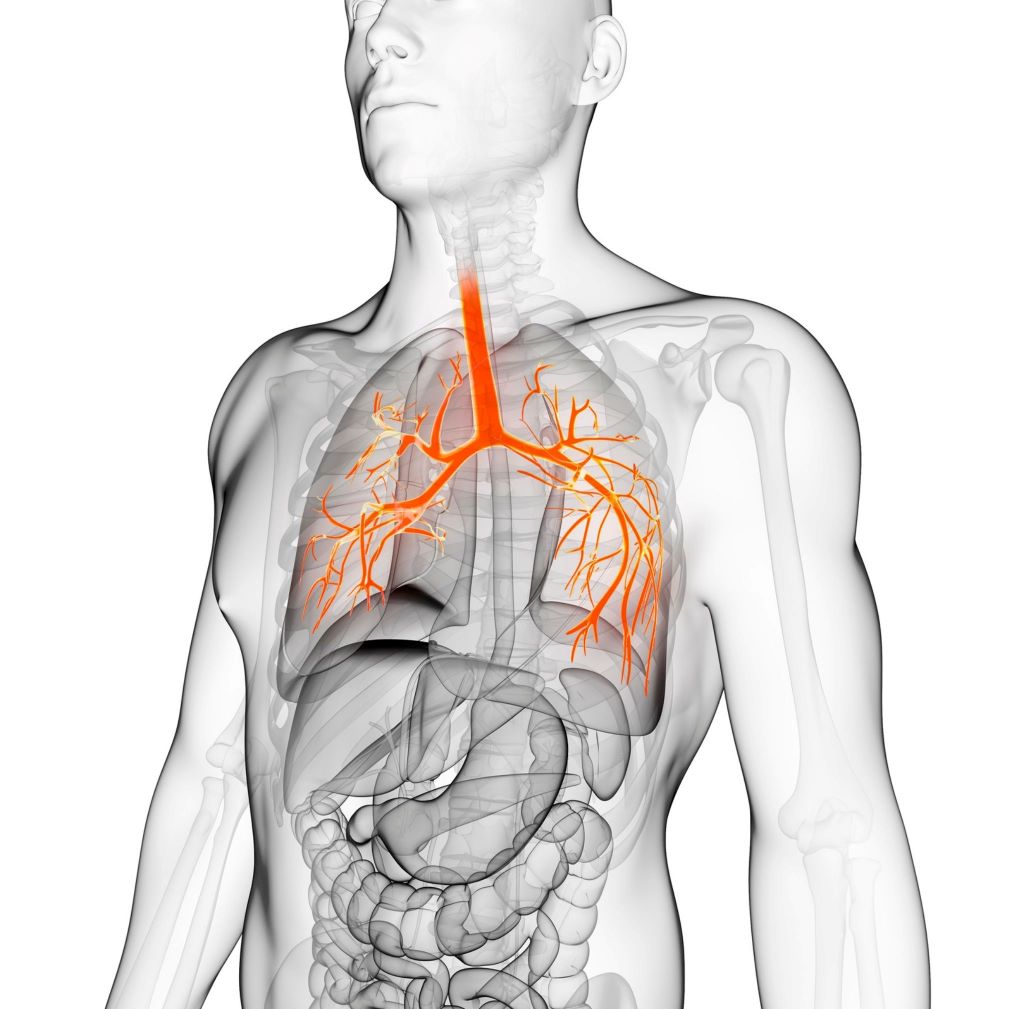
A pneumothorax, commonly known as a collapsed lung, is a medical condition that occurs when air accumulates in the pleural space surrounding the lung, causing lung compression and potential breathing difficulties. Timely and accurate diagnosis of a pneumothorax is crucial to ensure prompt medical intervention and prevent complications. In this comprehensive guide, we will explore the various methods and diagnostic tools used by healthcare professionals to identify and diagnose a pneumothorax.
1. Physical Examination:
The diagnostic process for a pneumothorax often begins with a thorough physical examination by a healthcare provider. During this examination, the physician will carefully listen to the patient’s lungs using a stethoscope. They will pay close attention to any abnormal breath sounds, such as decreased or absent breath sounds on the affected side, which may raise suspicion of a pneumothorax.
2. Chest X-ray:
One of the most common and initial diagnostic tests for a pneumothorax is a chest X-ray. X-ray images of the chest can help confirm the presence of a pneumothorax by revealing the accumulation of air in the pleural space. This radiographic evidence provides valuable information about the size and location of the collapsed lung, assisting in making an accurate diagnosis.
3. Computed Tomography (CT) Scan:
In some cases, a chest X-ray may not be sufficient to provide a complete evaluation of the pneumothorax. In such instances, a computed tomography (CT) scan is often recommended. A CT scan produces detailed cross-sectional images of the chest, providing a more comprehensive view of the lung and pleural space. It helps healthcare professionals better assess the extent and characteristics of the pneumothorax, as well as identify any underlying lung conditions that may contribute to the condition.
4. Ultrasound:
Ultrasound is another valuable imaging technique used in the diagnosis of a pneumothorax, particularly in emergency situations. It is a non-invasive and rapid method that can quickly identify the presence of air or fluid in the pleural space. Ultrasound is particularly useful for detecting even small pneumothoraces and can be performed at the patient’s bedside, providing real-time information for immediate decision-making.
5. Arterial Blood Gas (ABG) Analysis:
An arterial blood gas analysis is a blood test that measures the levels of oxygen and carbon dioxide in the blood. This test can provide important information about the patient’s respiratory status and gas exchange efficiency. In cases of pneumothorax, ABG analysis may reveal changes in blood gas levels due to reduced lung function. It aids in understanding the severity of the pneumothorax and helps guide the appropriate treatment plan.
6. Thoracentesis:
Thoracentesis is both a diagnostic and therapeutic procedure used in managing a pneumothorax. During thoracentesis, a thin needle or catheter is inserted through the chest wall to remove excess air or fluid from the pleural space. The collected sample can be analyzed to confirm the presence of a pneumothorax and determine its underlying cause. Additionally, thoracentesis may help relieve symptoms and improve lung function in certain cases.
7. Pleural Manometry:
Pleural manometry is a specialized procedure that measures the pressure within the pleural space. This procedure aids in differentiating between a simple pneumothorax and a tension pneumothorax, which is a more severe form of the condition. In a tension pneumothorax, air accumulates in the pleural space but cannot escape, causing increased pressure and compression of the lung and other mediastinal structures. Pleural manometry helps guide treatment decisions for tension pneumothorax.
8. Video-Assisted Thoracoscopic Surgery (VATS):
In certain situations where the diagnosis remains uncertain, or when a therapeutic intervention is required, video-assisted thoracoscopic surgery (VATS) may be recommended. VATS is a minimally invasive surgical procedure that involves inserting a tiny camera and surgical instruments into the chest through small incisions. It allows the surgeon to directly visualize the pleural space, identify the pneumothorax, and perform necessary treatments, such as lung re-expansion or pleurodesis.
Conclusion:
The accurate and timely diagnosis of a pneumothorax is essential in providing appropriate medical management and preventing potential complications. Healthcare professionals use a combination of physical examination, imaging studies like chest X-rays and CT scans, ultrasound, arterial blood gas analysis, and specialized procedures like thoracentesis and pleural manometry to diagnose a pneumothorax. Early diagnosis facilitates timely treatment, leading to improved patient outcomes and a quicker recovery.
If you suspect you have a pneumothorax or experience symptoms such as sudden chest pain, shortness of breath, or difficulty breathing, seek immediate medical attention. A healthcare professional, such as Dr. Mohan Venkatesh Pulle, can conduct a thorough evaluation and recommend the appropriate diagnostic tests to confirm the diagnosis and initiate the most suitable treatment.