What are the Different Stages of Esophageal Cancer?
Esophageal cancer is a formidable disease that affects the esophagus, the hollow tube that carries food and liquids...
+919999461292
MBBS | DNB (General Surgery, Gold Medalist) | DNB (Thoracic Surgery, Gold Medalist)
Thoracic & Lung Transplant Surgeon | Medanta – The Medicity, Gurugram

MBBS | DNB (General Surgery, Gold Medalist) | DNB (Thoracic Surgery, Gold Medalist)
Thoracic & Lung Transplant Surgeon | Medanta – The Medicity, Gurugram

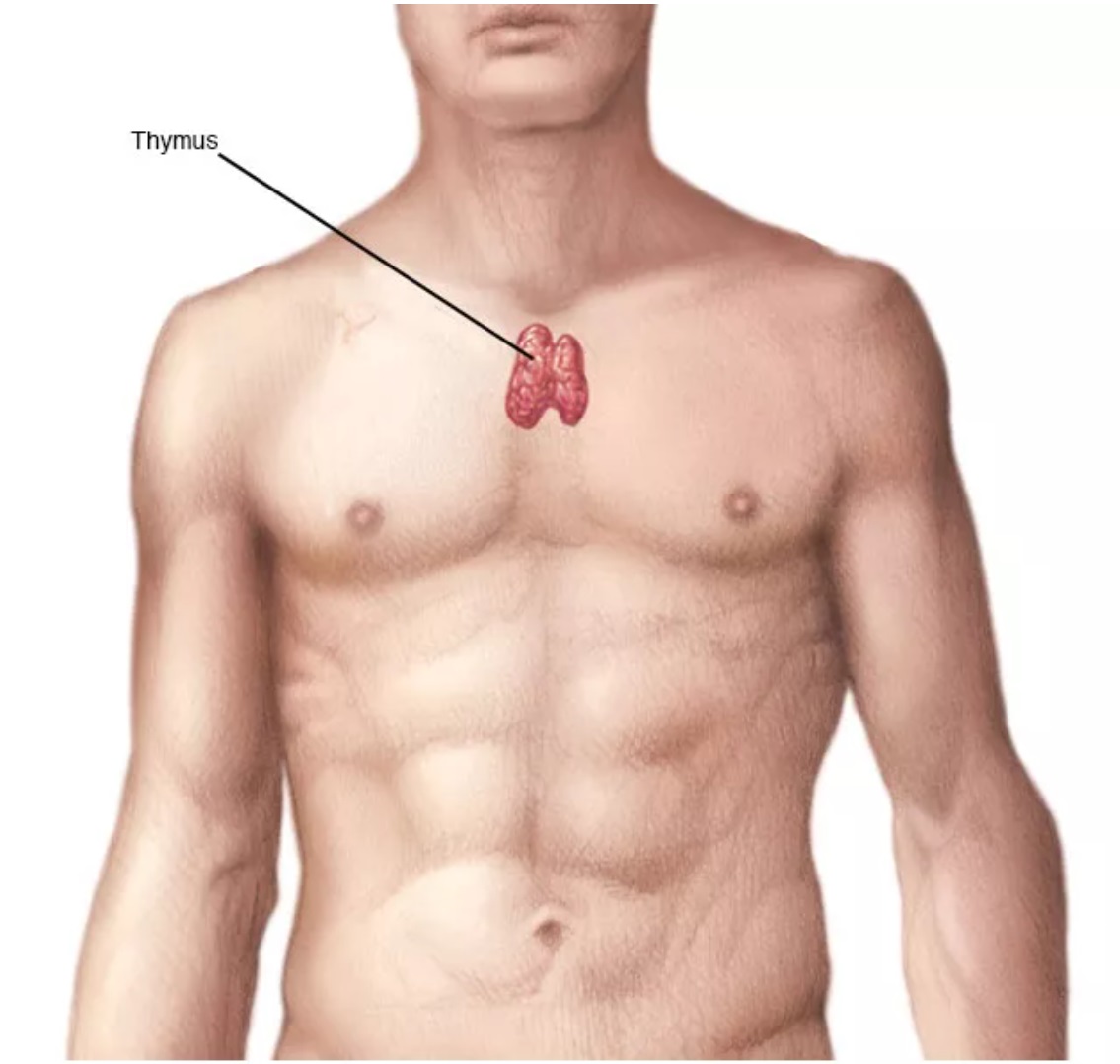
Thymoma is a rare type of tumor that originates in the thymus gland, which is a critical organ of the immune system located in the upper part of the chest, behind the sternum (breastbone). This gland plays a vital role in the development and maturation of T-lymphocytes (T cells), a type of white blood cell responsible for immune responses. Thymomas are part of a broader group of tumors known as thymic epithelial tumors, which also includes thymic carcinomas and thymic neuroendocrine tumors.
See, Thymoma is a tumor that develops in thymus gland, which is located in your chest, in front of the heart.. It’s usually slow-growing, but we need to treat it properly to prevent complications.
Not always. Many thymomas are benign, but some can be malignant. We’ll need to do proper tests to determine the exact nature of your tumor.
Interestingly, many patients don’t have symptoms. Sometimes people experience chest pain, cough, or breathing difficulty. Some patients develop autoimmune conditions like Myasthenia Gravis.
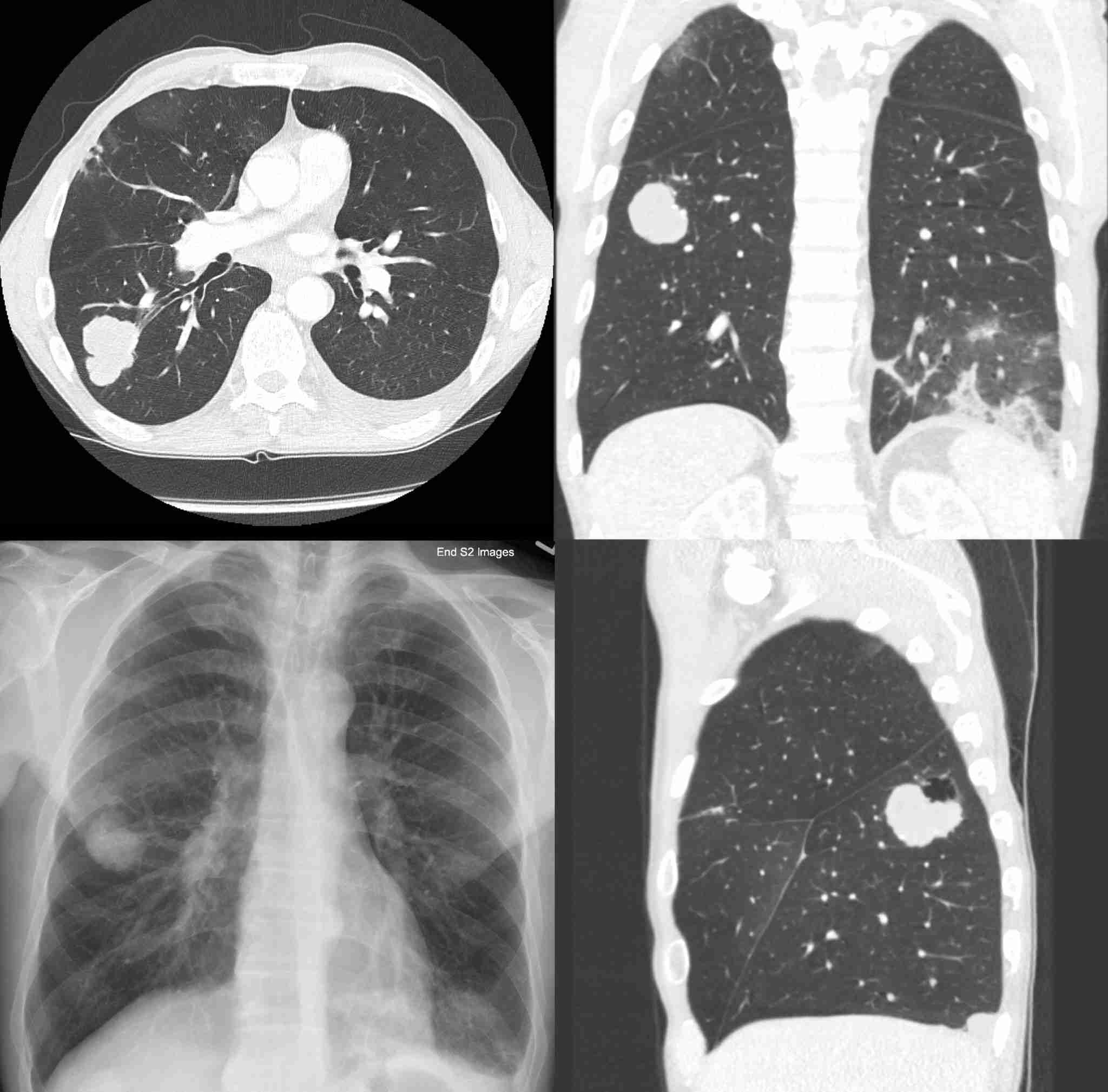
We usually start with chest X-ray, then do CT scan or MRI for detailed images. Sometimes we need to do a biopsy to confirm diagnosis. Don’t worry, we’ll guide you through the whole process.
Main treatment is surgery to remove the tumor. Surgery is “the” treatment for thymoma. Sometimes we combine it with radiation or chemotherapy, depending on stage and type.
In most cases, yes. Surgery gives best chance for complete removal of tumor. We usually do minimally invasive procedure called robotic surgery or VATS – small cuts only, faster recovery.
Like any surgery, there are some risks, but they’re generally low. Main ones are infection, bleeding, or damage to nearby structures. But don’t worry, we take all precautions to minimize risks.
Usually 3-5 days after VATS procedure. If we need to do open surgery, might be bit longer. But most patients recover quite quickly.
Depends on tumor stage and type. Sometimes we give these treatments before surgery to shrink tumor, sometimes after to prevent recurrence. We’ll decide best approach for your case.
Most patients return to normal activities in 3-4 weeks. But full recovery can take 2-3 months. We’ll give you proper instructions for gradual return to activities.
There’s small chance of recurrence, that’s why regular follow-up is important. We’ll monitor you closely with scans and check-ups.
Thymus gland is part of immune system, but in adults, its role is less critical. Removing it usually doesn’t cause significant immune problems. But we’ll monitor your health carefully
Light walking is good soon after surgery. Gradually increase activity over days. No heavy lifting for 6-8 weeks. We’ll give you proper exercise plan.
No strict diet restrictions, but healthy eating is important for recovery. Protein-rich foods help healing. Stay well hydrated. Our dietitian will give you proper guidance.
First year, every 3-4 months. Then twice a year for next 2-3 years. After that, yearly if everything stable. But if any new symptoms develop, contact us immediately.
Note: “Remember, every patient’s case is bit different. We’ll make treatment plan specific to your condition. My team and I are always here to support you through this journey.”
Thymoma is a rare type of tumor that originates in the thymus gland, which is a critical organ of the immune system located in the upper part of the chest, behind the sternum (breastbone). This gland plays a vital role in the development and maturation of T-lymphocytes (T cells), a type of white blood cell responsible for immune responses. Thymomas are part of a broader group of tumors known as thymic epithelial tumors, which also includes thymic carcinomas and thymic neuroendocrine tumors.

The thymus gland is most active during childhood and adolescence, after which it gradually diminishes in size and activity as a person reaches adulthood. During childhood, the thymus helps T cells develop and differentiate into mature cells with the ability to recognize and respond to foreign substances (antigens) in the body. These mature T cells then circulate in the bloodstream and lymphatic system, acting as crucial defenders against infections and cancer.
Thymomas are thought to arise from the epithelial cells of the thymus, which form the structure of the gland. While the exact cause of thymoma development is not fully understood, it is believed to involve genetic mutations that lead to uncontrolled cell growth.
Thymomas are classified based on their appearance and cellular characteristics under a microscope using the World Health Organization (WHO) classification system. There are different subtypes, ranging from type A, which tends to be less aggressive, to type AB, type B1, type B2, and type B3, with B3 being more aggressive. Thymic carcinoma is considered a separate and more aggressive entity than thymoma, as it has a higher potential for invasion and metastasis.
Thymomas are rare tumors, accounting for approximately 20% of all mediastinal tumors (tumors that occur in the middle of the chest). They are most commonly diagnosed in people between the ages of 40 and 60, but they can occur at any age. Thymomas are slightly more common in men than in women.
The underlying risk factors for thymoma development remain largely unknown, but there are some associations with specific conditions, such as myasthenia gravis (MG). MG is an autoimmune disorder in which the immune system attacks and weakens muscles, and it is found in about 30% of thymoma cases. Additionally, certain genetic syndromes, such as multiple endocrine neoplasia type 1 (MEN1), have been linked to an increased risk of thymomas.
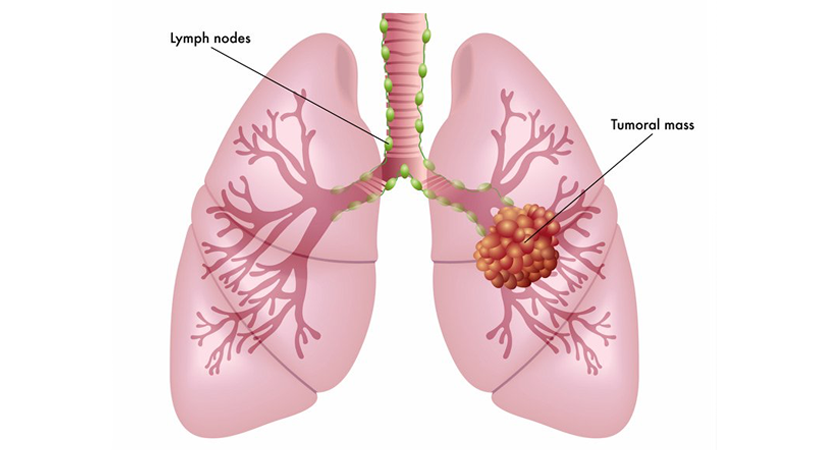
Thymomas often grow slowly, and in their early stages, they may not produce noticeable symptoms. As they enlarge, they can compress nearby structures in the chest, leading to various symptoms. Common signs and symptoms of thymomas include:
Diagnosing thymoma requires a comprehensive evaluation, including a detailed medical history, physical examination, and imaging studies. Chest X-rays, computed tomography (CT) scans, and magnetic resonance imaging (MRI) are commonly used to visualize the tumor and assess its size and location. Additionally, a biopsy is performed to obtain a tissue sample from the thymus for microscopic examination and classification.
Staging is a critical step in determining the extent and severity of thymoma. The most commonly used staging system for thymomas is the Masaoka staging system, which classifies thymomas into stages I, II, III, and IV based on tumor size and invasion of surrounding tissues. The higher the stage, the more extensive the tumor growth and spread.
The prognosis for thymoma varies depending on the tumor stage, histological subtype, and the presence of myasthenia gravis or other associated conditions. Generally, early-stage thymomas (stage I and II) have a more favorable prognosis, while advanced-stage thymomas (stage III and IV) tend to have a lower survival rate. However, each case is unique, and survival outcomes can be influenced by various factors, including the effectiveness of treatment and the patient’s overall health.
The treatment of thymoma is tailored to the individual patient and depends on the tumor stage, histological subtype, and the presence of associated conditions. The main treatment options for thymoma include:
– Surgery: Surgical removal of the thymoma is the primary treatment for early-stage tumors. In some cases, complete surgical resection can lead to a cure.
– Radiation Therapy: Radiation therapy may be used after surgery to target any remaining cancer cells or as the primary treatment for unresectable tumors.
– Chemotherapy: Chemotherapy may be employed for advanced-stage thymomas or those that have spread beyond the thymus.
– Targeted Therapy: In some cases, targeted therapies that specifically target certain molecules or pathways involved in thymoma growth may be used.
– Immunotherapy: Immunotherapy, including checkpoint inhibitors, has shown promise in treating some types of thymomas.
– Multimodal Approaches: Depending on the case, a combination of surgery, radiation therapy, and chemotherapy may be used to improve treatment outcomes.
After treatment, regular follow-up visits with the healthcare team are essential to monitor for any signs of recurrence and manage potential long-term effects of treatment. Follow-up care may include physical exams, imaging studies, and blood tests to assess the patient’s health and detect any changes.
As thymomas are relatively rare, there is ongoing research aimed at better understanding the biology of these tumors and developing more effective treatment approaches. Clinical trials play a crucial role in testing new treatments and therapies for thymomas, potentially leading to improved outcomes for patients in the future.
Esophageal cancer is a formidable disease that affects the esophagus, the hollow tube that carries food and liquids...
Esophageal cancer is a formidable and often challenging disease that affects the esophagus, the muscular tube that carries...
Esophageal cancer is a challenging and potentially life-threatening condition that requires timely diagnosis and appropriate treatment. When esophageal...
Esophageal cancer is a serious and potentially life-threatening disease that affects the esophagus, the muscular tube that carries...
Esophageal cancer is a formidable adversary that can silently develop within the esophagus, the muscular tube connecting the...
Esophageal cancer is a serious and potentially life-threatening condition that affects the esophagus, the muscular tube responsible for...
WhatsApp us