Aspergilloma: Understanding Fungal Ball in the Lungs
An aspergilloma, also known as a mycetoma or fungal ball, is a unique and distinct form of pulmonary (lung) infection caused by the fungus Aspergillus. Unlike typical lung infections, an aspergilloma does not invade lung tissues but forms a ball-like structure within pre-existing lung cavities or damaged airspaces. This condition predominantly affects individuals with underlying lung diseases, such as tuberculosis or bronchiectasis, and understanding its pathogenesis, clinical presentation, diagnosis, and treatment is crucial for managing this challenging condition effectively.
1. The Aspergillus Fungus:
Aspergillus is a common fungus found in the environment, including soil, decaying vegetation, and compost piles. It can also be present in indoor environments. While most people inhale Aspergillus spores without any health consequences, individuals with weakened immune systems or underlying lung diseases are at risk of developing Aspergillus-related conditions, including aspergilloma.
2. Pathogenesis of Aspergilloma:
Aspergilloma usually occurs in individuals with pre-existing lung cavities or damaged lung tissues. Common underlying conditions associated with aspergilloma include:
– Pulmonary Tuberculosis: Individuals who have had tuberculosis in the past may develop lung cavities as a result of the disease. These cavities provide an ideal environment for Aspergillus spores to colonize and form fungal balls.
– Bronchiectasis: Bronchiectasis is a condition characterized by the permanent dilation of the bronchi (airways) due to chronic inflammation or infection. The damaged airways can trap Aspergillus spores and contribute to aspergilloma formation.
– Other Lung Diseases: Conditions such as chronic obstructive pulmonary disease (COPD), sarcoidosis, and lung abscesses can also create spaces or cavities in the lungs, facilitating the development of aspergilloma.
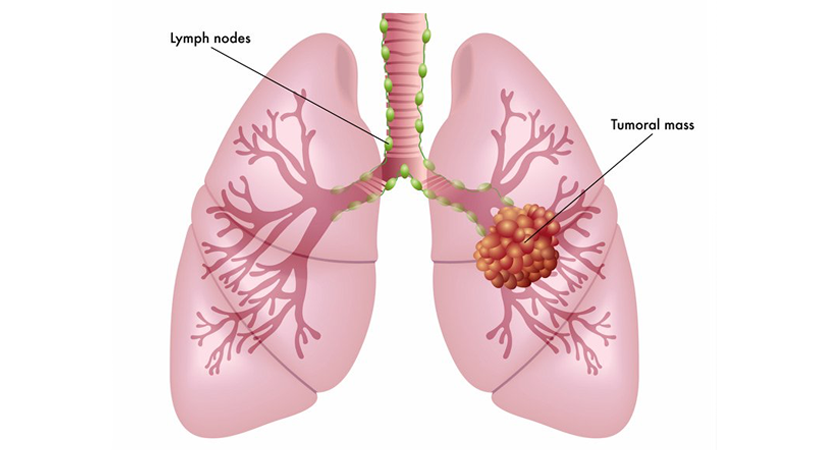
3. Formation of Aspergilloma:
When individuals with lung cavities or damaged airspaces inhale Aspergillus spores, the fungus can colonize these spaces and grow as a mass of fungal hyphae (thread-like structures). Over time, this mass of hyphae becomes surrounded by a conglomeration of mucus, fibrin, and inflammatory cells, forming a ball-like structure known as the aspergilloma. This ball of fungus and debris is typically referred to as the “fungus ball.”

4. Clinical Presentation:
Aspergilloma can remain asymptomatic in some cases and may be incidentally detected during chest imaging for other medical reasons. However, symptomatic individuals may present with the following:
– Hemoptysis: Coughing up blood is the most common and concerning symptom of aspergilloma. The fungus ball can erode the blood vessels within the lung cavity, leading to intermittent or persistent hemoptysis.
– Chronic Cough: A persistent cough may be present, accompanied by mucus production.
– Chest Pain: Some individuals may experience chest pain, which can result from inflammation or irritation of the surrounding lung tissues.
– Recurrent Respiratory Infections: Aspergilloma can make affected individuals more susceptible to respiratory infections, leading to recurrent pneumonia or exacerbations of underlying lung diseases.
5. Diagnosis:
The diagnosis of aspergilloma involves a combination of clinical evaluation, chest imaging, and laboratory tests. Diagnostic steps include:
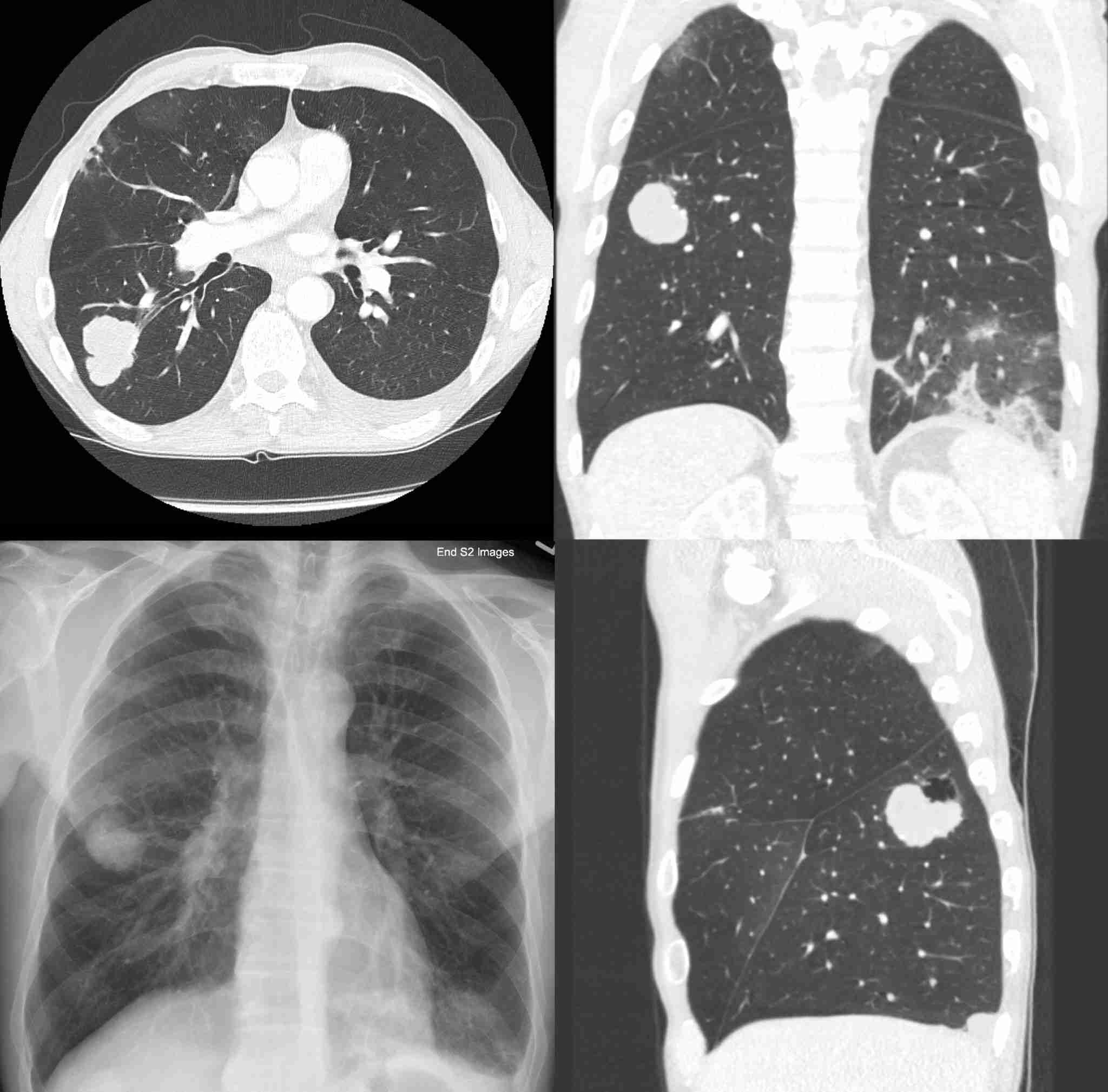
– Chest X-ray: Initial imaging may reveal a round or oval-shaped mass within a lung cavity.
– Computed Tomography (CT) Scan: CT scan is the most sensitive imaging modality for detecting aspergillomas. It can provide detailed images of the fungal ball and its relationship with surrounding lung tissues.
– Sputum Examination: Sputum samples may be examined for the presence of Aspergillus spores, but this test alone is not definitive for diagnosing aspergilloma.
– Bronchoscopy: Bronchoscopy may be performed to directly visualize the airways and confirm the presence of the aspergilloma. During bronchoscopy, a flexible tube with a camera is inserted into the airways, allowing the physician to view the fungal ball and collect samples for further testing.
6. Treatment Options:
The management of aspergilloma depends on the severity of symptoms, the size and location of the fungal ball, and the overall health of the affected individual. Treatment options include:
– Observation: Asymptomatic individuals or those with mild symptoms may be managed with observation and regular monitoring.
– Antifungal Medications: Antifungal drugs, such as itraconazole or voriconazole, may be prescribed to control the growth of Aspergillus and prevent the progression of the aspergilloma. However, these medications do not eliminate the existing fungal ball.
– Bronchial Artery Embolization: For individuals with severe hemoptysis, bronchial artery embolization may be performed to block the blood supply to the aspergilloma, reducing the risk of bleeding.
– Surgical Intervention: Surgical removal of the aspergilloma may be considered in certain cases, especially if it is causing life-threatening hemoptysis or significantly compromising lung function. Surgical options include wedge resection or segmentectomy, aiming to remove the affected lung tissue while preserving as much healthy lung as possible.
7. Prognosis and Complications:
The prognosis for aspergilloma varies depending on the extent of the disease and the effectiveness of treatment. Asymptomatic or minimally symptomatic individuals may have a good prognosis with conservative management. However, severe hemoptysis and recurrent infections can be life-threatening and may require urgent intervention.
8. Prevention and Risk Reduction:
Preventing aspergilloma involves managing the underlying lung conditions that create spaces or cavities where the fungus can colonize. Effective management of conditions such as tuberculosis, bronchiectasis, and other lung diseases can reduce the risk of aspergilloma formation.
9. Emerging Therapies and Research:
Research continues to explore new approaches for the management of aspergilloma. Some studies are investigating the use of minimally invasive techniques and advanced antifungal therapies to improve patient outcomes.
10. Education and Awareness:
Awareness of aspergilloma and its risk factors is essential among healthcare providers and individuals with underlying lung conditions. Early detection and intervention can help prevent complications and improve the quality of life for affected individuals.
Related Articles
edit post
Esophageal Cancer
What are the Different Stages of Esophageal Cancer?
Esophageal cancer is a formidable disease that affects the esophagus, the hollow tube that carries food and liquids…
edit post
Esophageal Cancer
What are the Treatment Options for Esophageal Cancer?
Esophageal cancer is a formidable and often challenging disease that affects the esophagus, the muscular tube that carries…
edit post
Esophageal Cancer
How is Esophageal Cancer Diagnosed and Treated When It Originates in the Posterior Mediastinum?
Esophageal cancer is a challenging and potentially life-threatening condition that requires timely diagnosis and appropriate treatment. When esophageal…
edit post

Esophageal Cancer
How is Esophageal Cancer Diagnosed? A Comprehensive Guide
Esophageal cancer is a serious and potentially life-threatening disease that affects the esophagus, the muscular tube that carries…
edit post
Esophageal Cancer
What are the symptoms of Esophageal Cancer? : A Comprehensive Guide to its Symptoms
Esophageal cancer is a formidable adversary that can silently develop within the esophagus, the muscular tube connecting the…
edit post

Esophageal Cancer
What is Esophageal Cancer, and What Are Its Types?
Esophageal cancer is a serious and potentially life-threatening condition that affects the esophagus, the muscular tube responsible for…

